As healthcare and public health strategists, we at Ascendient spend a lot of time thinking about possible changes in the external environment – and how those changes might affect our clients. That’s serious work, but this time of year offers the chance to have a little fun with it.
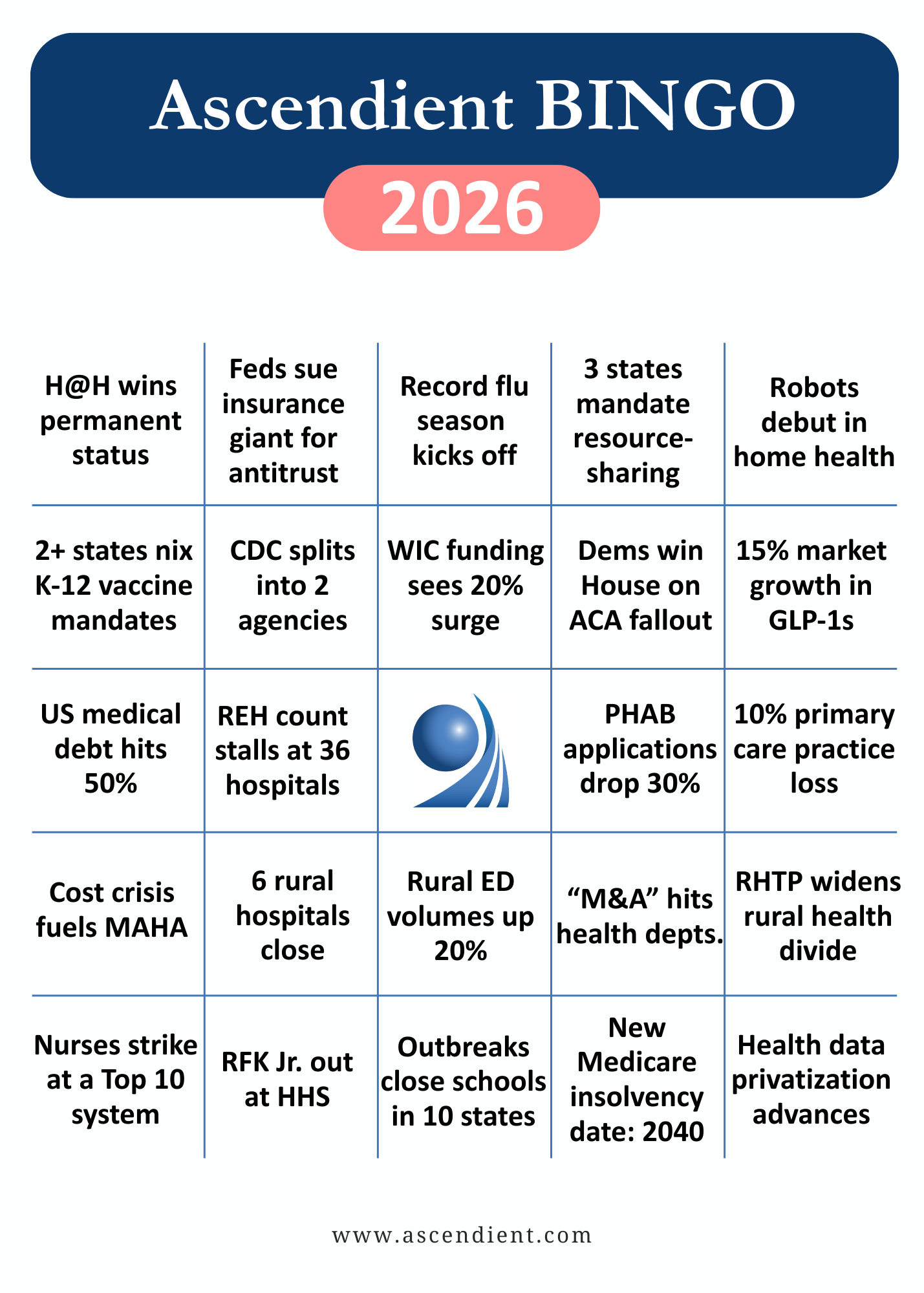
At our recent holiday get-together, I invited the Ascendient team to share their most salient predictions for 2026. With some light editing, we’ve pulled those together into our first-ever New Year’s Bingo Card.
These are not the firm’s “official” positions, by any means. As senior partner, I don’t agree with the timing or intensity of every prediction, but I think you’ll agree the logic is compelling, and I hope the Bingo card will get your own creative juices flowing.
What did we miss? What did we get wrong? Feel free to add your comments on this LinkedIn post, and we’ll check back mid-year with a progress report. Happy New Year!
1. Hospital at Home wins permanent status – With cost savings and reduced admissions, the business case for Hospital at Home is overwhelming – plus, the model offers a solution to the workforce and hospital capacity crunch. By the third quarter of 2026, Congress will end the ongoing waiver whiplash with legislation that makes Medicare reimbursement permanent. Expect health insurers (who already have care management infrastructure and member data) to partner with or acquire Hospital at Home platforms, while PE-backed pure-plays aggressively scale up. Meanwhile, health systems that waited for "proof of concept" will find themselves behind the curve. – Laura Armstrong-Brauer
2. Feds sue insurance giant for antitrust – The large insurance companies are getting more powerful as they accelerate their vertical integration strategy of combining their payer, pharmacy, and provider networks. Public backlash could cause the federal government to begin antitrust actions against one of the big players to appease voters. – Fred Sanders
3. Record flu season kicks off – For the 2026 flu season, which starts in October, deaths are likely to be the highest in decades. Worsened in part by anti-vaccine sentiment from HHS leadership, vaccination rates have been decreasing, including an estimated 12% decline in flu shots from 2024 to 2025. – Paul Riker
4. Three states mandate resource-sharing between health systems and health departments – With public health facing severe staffing shortages, at least three states will require hospitals and health systems to share specialized personnel (such as epidemiologists, nurses, or laboratory staff) with understaffed health departments. Governors will frame these mandates as mutual benefit arrangements where hospitals gain enhanced disease surveillance and outbreak intelligence while sustaining the public health infrastructure that manages communicable disease control and prevents emergency department surges. – Kelly Conley
5. Robots make home care debut – I think we’ll see the premier of NEO Personal Care Assistants by the end of 2026. Several Japanese companies have already deployed humanoid robots to assist with eldercare in Japan, driven by many of the same pressures we see here: high cost and low availability of in-facility care; a severe lack of personal care workers for either in-home care or in-facility care; and a burgeoning elder population in need of services. – Dawn Carter
6. Two or more states nix K-12 vaccine mandates – Florida showed the way in 2025, and the issue is already percolating in other red states where legislators are finding political cover in the synergy of parental rights messaging, social media amplification, and tacit federal approval. This isn't just policy change – it's a stress test of herd immunity thresholds in real-time. We may see measles or pertussis outbreaks that force a reversal, making this a high-stakes natural experiment. – Laura Armstrong-Brauer
7. CDC splits into two agencies – The Administration for a Healthy America will officially launch in 2026, absorbing CDC's chronic disease, environmental health, and injury prevention programs. This restructuring – combined with 20% workforce reductions and the relocation of Atlanta-based expertise to Washington – will create a divided system where disease surveillance operates separately from health promotion, fundamentally altering how federal public health expertise flows to state and local departments. – Chelsey Saari
8. WIC funding sees 20% surge – Bipartisan concern about infant mortality and compelling economic data showing every WIC dollar saves $1.77 to $3.13 in healthcare costs (and up to $2.48 when including educational and productivity savings over a lifetime) will drive appropriations to an unprecedented $9.1 billion, a 20 percent increase over current funding. With food costs up 24% since 2020 and growing evidence that WIC prevents costly preterm births and chronic conditions, Congress will frame this historic investment as both inflation adjustment and long-term fiscal strategy, making it a rare consensus issue defensible across the political spectrum. – Kelly Conley
9. Dems win house on ACA fallout – The end of ACA subsidies will increase the number of uninsured Americans. Since the typical ACA purchaser is a white male living in a rural area in a red state this could increase the likelihood of a shift in the majority in Congress potentially on the scale of the 1994 midterm election, when the Republican Party gained unified control for the first time since 1952. Ironically, Bill (And Hillary) Clinton’s universal healthcare proposals were one of the reasons voters turned from the Democratic Party that year. – Fred Sanders
10. 15% market growth in GLP-1s – The global GLP-1 weight loss market will grow at least 15% by the end of 2026 as prices decline and access expands. A major catalyst will be Eli Lilly’s first true oral GLP-1, expected in March 2026, which should significantly improve adherence and broaden the patient base for obesity treatment. Additional momentum will come from the expiration of active-ingredient patents in several countries, including China, beginning in March 2026, opening the door for generic competition and further accelerating market adoption. – Rachel Short
11. US medical debt hits 50% – A 2022 KFF analysis found that 41% of American adults had some type of healthcare debt, when including debt carried on credit cards or owed to family members. With ACA healthcare subsidies and Medicaid coverage in flux and broader consumer economic concerns in play, I predict that that 41% estimate will increase sharply, particularly among Boomers and those who benefited most from Medicaid expansion. – Emily McCallum
12. REH count stalls at 36 hospitals – Despite 300+ hospitals at "immediate risk" of closure, the 36 REHs operating since 2023 will remain the total through 2026 as Congress is paralyzed on fixes needed to make conversion viable. Even bills with bipartisan backing have stalled in committee for months with no movement, while healthcare policy debates focus on ACA subsidies and implementing OBBBA's $1 trillion Medicaid cuts. With structural barriers unaddressed and Congress gridlocked, struggling hospitals will choose closure or acquisition over a model with unresolved economics. – Allison Cooper
13. FREE
14. PHAB (re)accreditation applications drop 30% – A combination of severe workforce shortages, leadership turnover, and budget uncertainty will cause health departments to deprioritize voluntary accreditation with the Public Health Accreditation Board. With quality improvement coordinators being among the first positions cut and reaccreditation cycles requiring substantial staff time, departments will shift focus to basic service delivery over quality improvement infrastructure, effectively reversing a decade of professionalization efforts. – Chelsey Saari
15. 10% primary care practice loss – Medicare reimbursement cuts combined with rising operational costs will make traditional primary care economically unviable, driving practice closures, early retirements, and conversions to concierge models—particularly in non-Medicaid expansion states where uninsured patient loads strain already thin margins. Medical students increasingly avoid primary care specialties, while mid-career physicians in affluent markets discover they can earn more while seeing fewer patients under subscription models. The result: a 10% net reduction in traditional primary care availability, hitting hardest in areas that can least afford to lose access. – Jeff Stofko
16. Cost crisis fuels MAHA – Rising healthcare costs and insurance premiums will push more Americans to embrace MAHA principles that refocus U.S. health priorities on prevention and lifestyle-based strategies. As consumers seek cheaper alternatives to insurance-backed care, routine primary care utilization will decline while spending on wellness and non-clinical lifestyle medicine will grow. This cost-driven overcorrection will reduce adherence to proven public health and medical interventions, worsening public health outcomes despite higher individual spending on wellness. – Rachel Short
17. Six rural hospitals close – Four rural hospitals shut down completely last year, according to the Sheps Center at UNC, but that number will likely rise by 50% in 2026 due to deep Medicaid cuts. If Congress finds a fix for the Rural Emergency Hospital model (stepped-up reimbursement is currently limited to Medicare, not Medicaid), rural closures for 2026 could drop to zero, but political consensus looks unlikely. – Robert Jones
18. Rural ED volumes up 20% – When ACA subsidies expire in January 2026, 4 million Americans will lose coverage, with rural populations in non-Medicaid expansion states hit hardest. Rural EDs, already operating on razor-thin margins, will see 20% volume increases as uninsured patients defer care until conditions become emergent and EMTALA obligations force treatment. With limited urgent care alternatives and years of hospital closures having already gutted safety-net capacity, surviving rural EDs will face unsustainable uncompensated care burdens that could trigger a new wave of closures before year-end. (See prediction #17.) – Jeff Stofko
19. RFK Jr. out at HHS – As healthcare costs continue to rise, Republicans will become increasingly vulnerable to the Democrats’ advantage on the “cost of living” issue, and Kennedy might be a convenient scapegoat. In addition, with Musk gone, Kennedy is the biggest celebrity still in Trump’s cabinet – and the president is not known for sharing the spotlight. – Robert Jones
20. RHTP widens rural health divide – All 50 states applied for Rural Health Transformation Program funding, but the program only continues to release dollars after a state hits performance milestones within 24 months. This rewards states with existing transformation capacity while penalizing those still building it. States with proven methodologies can iterate on success, but those lacking capacity will miss early marks and face funding clawbacks when most needed. The weakest states face a double blow: RHTP funding reductions alongside massive Medicaid cuts they're least equipped to absorb. – Allison Cooper
21. Nurses strike at a Top 10 health system – There were multiple high-profile nurses’ strikes across US hospitals in 2025, including the Kaiser Permanente system in California. The trend is likely to accelerate in 2026 as the economy stagnates and AI proliferates without sufficient buy-in from the existing workforce. – Paul Riker
22. “M&A” hits public health departments – Consolidation isn't just for hospitals anymore. As resources are cut, local health departments (especially in fragmented systems like NJ) will need to merge for regional models to still be able to provide comprehensive public health services. – Patricia Dowbiggin
23. Vaccine-preventable disease outbreaks close schools in 10 states – Immunization rates have fallen below herd immunity thresholds in over 30 states, with kindergarten vaccination coverage at 92.7 percent nationally. When measles requires 95 percent coverage to prevent community spread, we are living on borrowed time. Expect 2026 to bring simultaneous regional outbreaks forcing school closures of 2-3 weeks in at least 10 states as districts struggle to contain transmission among unvaccinated student populations. – Kelly Conley
24. New Medicare insolvency date: 2040 – The projected insolvency date for Medicare’s Hospital Insurance Trust Fund is always a moving target. Over just the past three years, the Medicare Trustees Report has cited a date of 2031, then 2036, and most recently 2033. This year – just in time for the mid-term elections – I think we’ll see a record “improvement,” with insolvency pushed all the way out to 2040 and lots of messaging around reductions in “waste, fraud, and abuse.” – Robert Jones
25. Health data privatization advances – From the Census Bureau to the CDC, we watched federal data disappear last year. In 2026, private health systems, insurers, and data aggregators will attempt to fill the gap – but at a cost. Expect proprietary datasets to become a competitive advantage. As health research gets more expensive and less transparent, academic researchers and smaller health systems could get priced out. There's also real risk of "data shopping," where politically aligned sources cherry-pick metrics. – Laura Armstrong-Brauer










